Plantar Fasciitis Treatment in Chicago
Ravenswood Chiropractic in Chicago Uses Advanced Technologies for providing Quick Relief from Plantar Fasciitis Pain.
Our Chicago clinic utilizes advanced technologies and the newest science-based, evidence-based treatment methods to quickly and effectively promote healing and relieve plantar fasciitis pain. These include radial shockwave therapy, physical therapy, extremity adjustments, and custom foot orthotics. Our clinic also offers other supportive treatments such as acupuncture, massage, and ice therapy to reduce inflammation and pain from trusted and experienced experts.
-
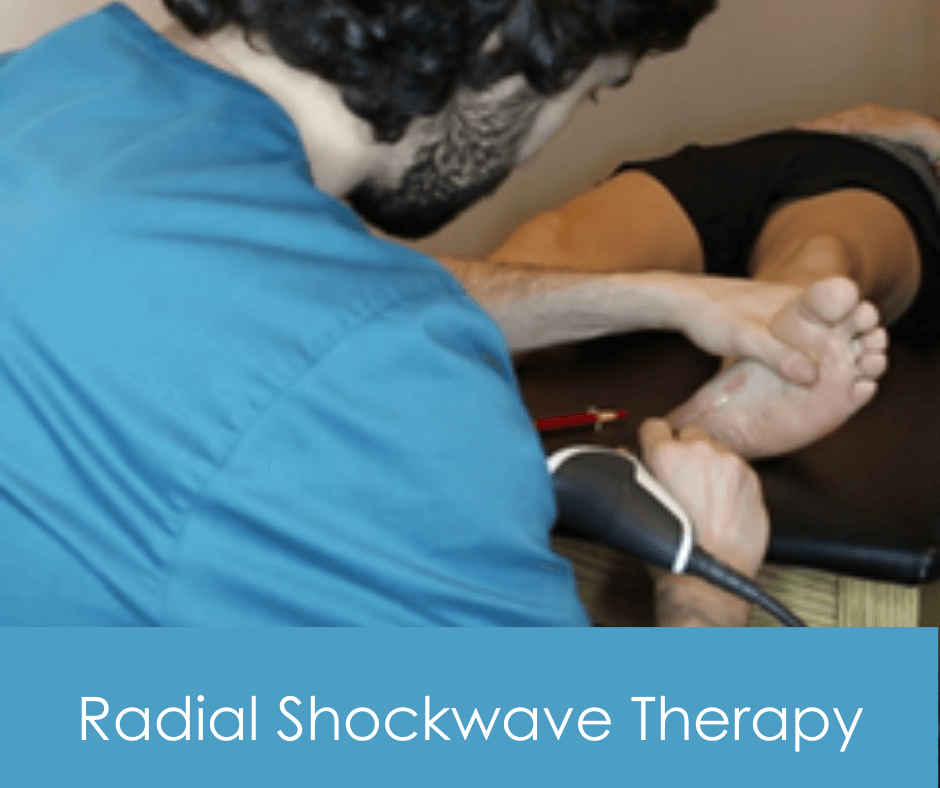
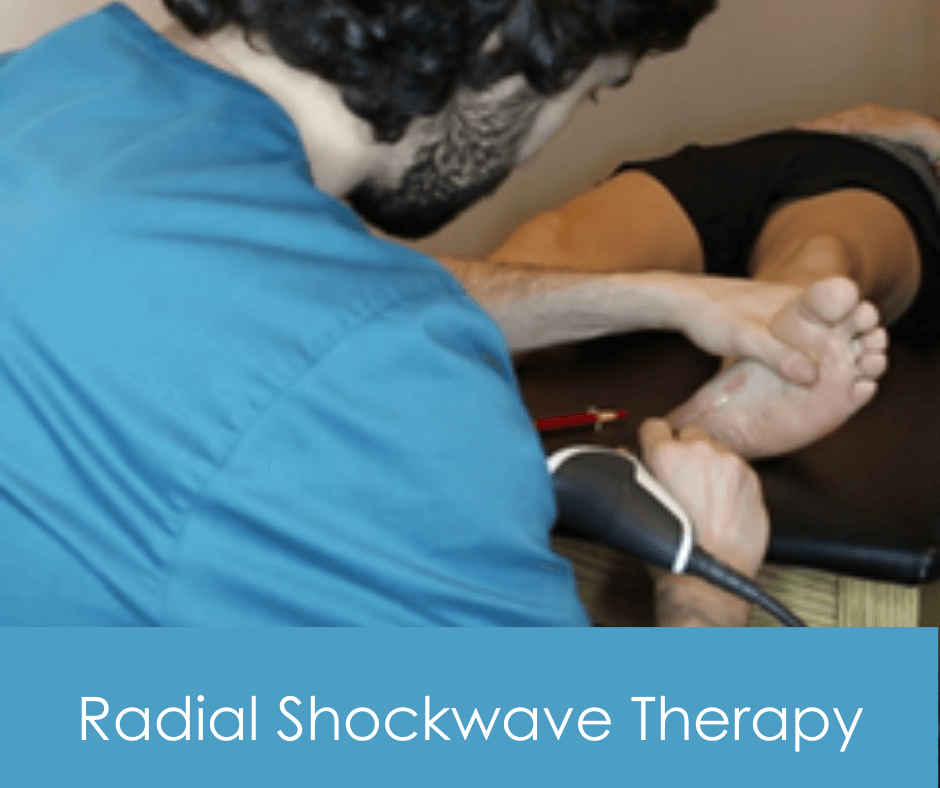
Radial Shockwave Therapy
Radial shockwave therapy is an increasingly popular technique used to treat persistent plantar fasciitis pain at Ravenswood Chiropractic in Chicago. This safe, non-invasive treatment uses sound waves that are sent directly into the heel or foot, that stimulate healing by accelerating procollagen synthesis and improving blood circulation to the injured area. This is important because the latest research suggests that plantar fasciitis is caused by collagen degeneration. Radial Shockwave therapy also has a high success in reducing the pain of plantar fasciitis by dispatching pain mediator Substance P with it’s sound waves. Studies have found that this therapy reduces inflammation by stimulating mast cell activity and improves healing time. Additionally, it can release tight muscles and tendons to reduce your foot pain and may even provide long-term relief from chronic heel discomfort. Treatments last 5-10 minutes and are scheduled a week apart.
-
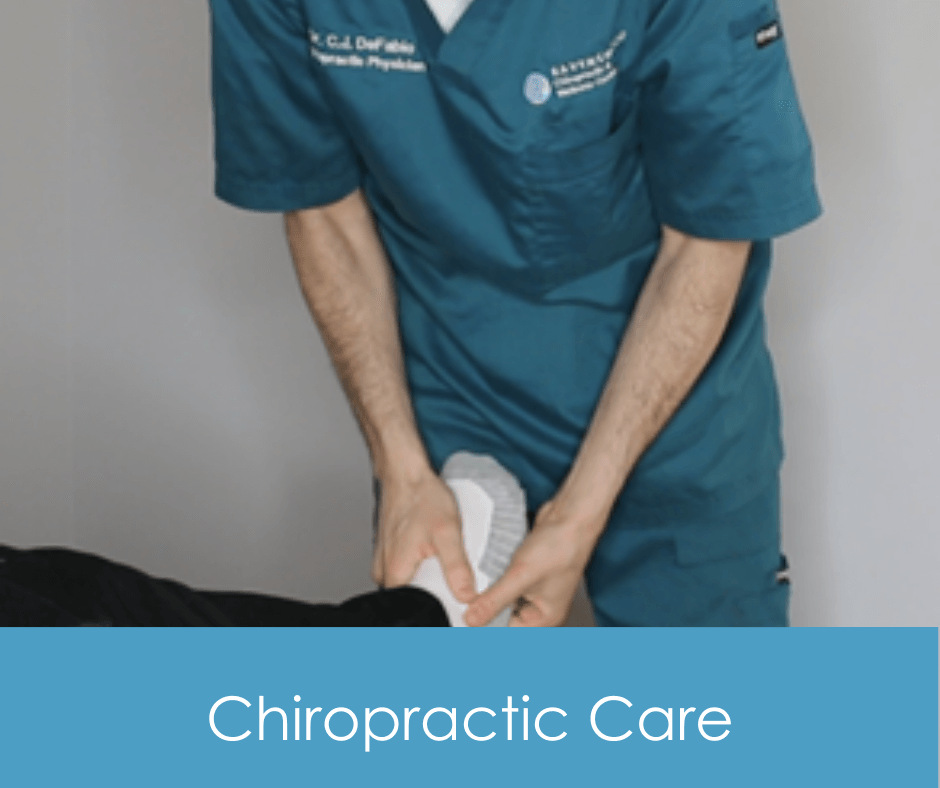
Chiropractic
One of the best things you can do especially if your plantar fasciitis is chronic, recurrent or has failed to respond to other conservative care, is to get an examination by a chiropractor who is skilled in Functional Assessment to see if there are any biomechanical issues placing stress on your plantar fascia. If stressors are identified, they can usually be easily addressed with chiropractic care and your plantar fasciitis symptoms resolved.
-

Physical Therapy
Stretching is one of the key components in plantar fasciitis treatment. It helps relax the muscles, improve blood circulation and reduce tightness in your leg muscles and the arch of your foot. Regular stretching can also help keep your foot strong, flexible, and less prone to future flare-ups.
-

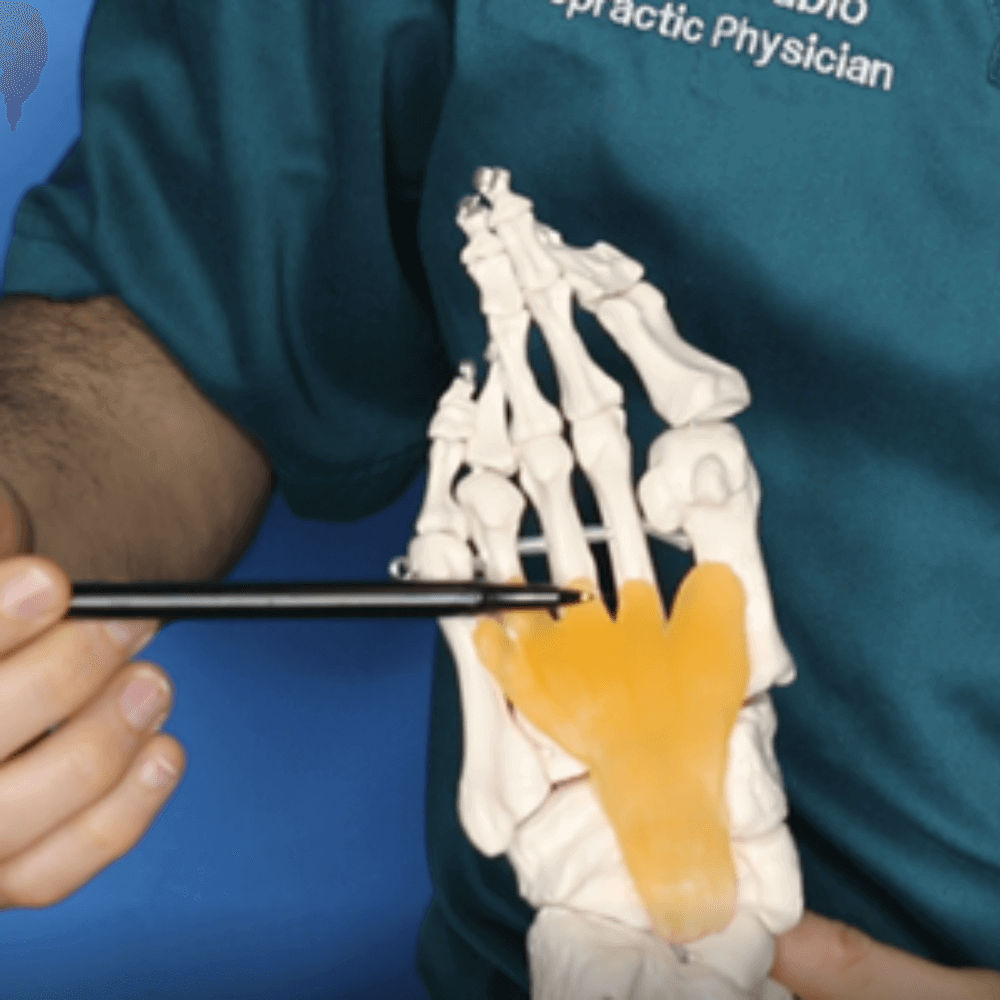
Acupuncture
We have also seen much success using acupuncture and gua sha for the treatment of plantar fasciitis. To treat plantar fasciitis, our acupuncturist will most likely focus on a point located in the center of your heel known as Shimian M-LE-5. Electroacupuncture needles may be used in conjunction with standard acupuncture needles. Other acupuncture points along the kidney and bladder channels have also been shown to be effective in treating plantar fasciitis.
Just as our massage therapy team would also focus on leg muscles to help plantar fasciitis symptoms, so too will our acupuncturist. Acupuncture points along the back of the calf muscles may also be targeted to help reduce strain on the plantar fascia. Finally, our acupuncturist may determine that targeting other channels that help balance the qi and blood flow to certain organs will help heal your foot arch pain.
-

Massage
At Ravenswood Chiropractic and Wellness Center we have found massage therapy especially helpful for treating the symptoms of plantar fasciitis. By incorporating myofascial release or deep tissue massage into your plantar fasciitis treatment routine, our team can focus directly on the tissue that is causing the pain. By focusing on the fascia itself, the Achilles heel, and even the calf muscles in the leg, deep tissue massage and myofasical release can relieve muscle tension and help to break up scar tissue and adhesions that can develop over time.
Our expert team can help you decide if deep tissue massage or myofascial release is right for your plantar fasciitis treatment. Even after performing treatment in our office, our massage therapist can teach you self-massage techniques to do at home between visits to help you feel better faster.
-

Custom Orthotics
Custom orthotics can become essential in your struggle against plantar fasciitis if you have flat feet or fallen | falling arches or another biomechanical issue. Custom orthotics work much differently than store bought inserts (which we typically do not recommend). When your arch drops, or begins to drop, the plantar fascia begins to tear away from your calcaneal (heel). Custom orthotics are specially fitted by our chiropractor in our office to your actual feet and are specially designed by the lab at Sole Supports (also used by professional athletic teams and Olympic athletes) to correct your arch as well as completely support it. This support results in reduced stress, halts the process, and allows it time to heal. Many of our patients who receive Sole Supports custom orthotics to correct biomechanical causes of their plantar fasciitis experience a 50-70% reduction of symptoms in 1 month, 70-90% at 2 months, and 90-100% at 3 months. Continued use of our custom orthotics often prevents recurrence of plantar fasciitis.